A dislocated shoulder is a common yet painful injury that occurs when the head of your upper arm bone (humerus) completely separates from the socket of your shoulder blade (glenoid). This often occurs due to a sudden impact, a fall, or a forceful twisting motion.
Understanding the signs and symptoms of a dislocated shoulder is important for prompt medical attention and effective treatment. In this post, we’ll take a closer look at shoulder dislocations, covering everything from their causes and symptoms to various treatment options and the rehabilitation process.
Key Takeaways
- A dislocated shoulder may present with intense pain, a visibly deformed appearance, and a limited range of motion.
- Dislocations commonly result from trauma such as falls, sports injuries, or motor vehicle accidents. However, individuals with pre-existing shoulder instability may experience dislocations from less significant forces.
- Treatment ranges from non-surgical methods like closed reduction, immobilization, and physical therapy to surgical interventions.
- A structured rehabilitation program involving physical therapy typically plays an important role in restoring range of motion, strength, and stability to the shoulder.
What is a Dislocated Shoulder?
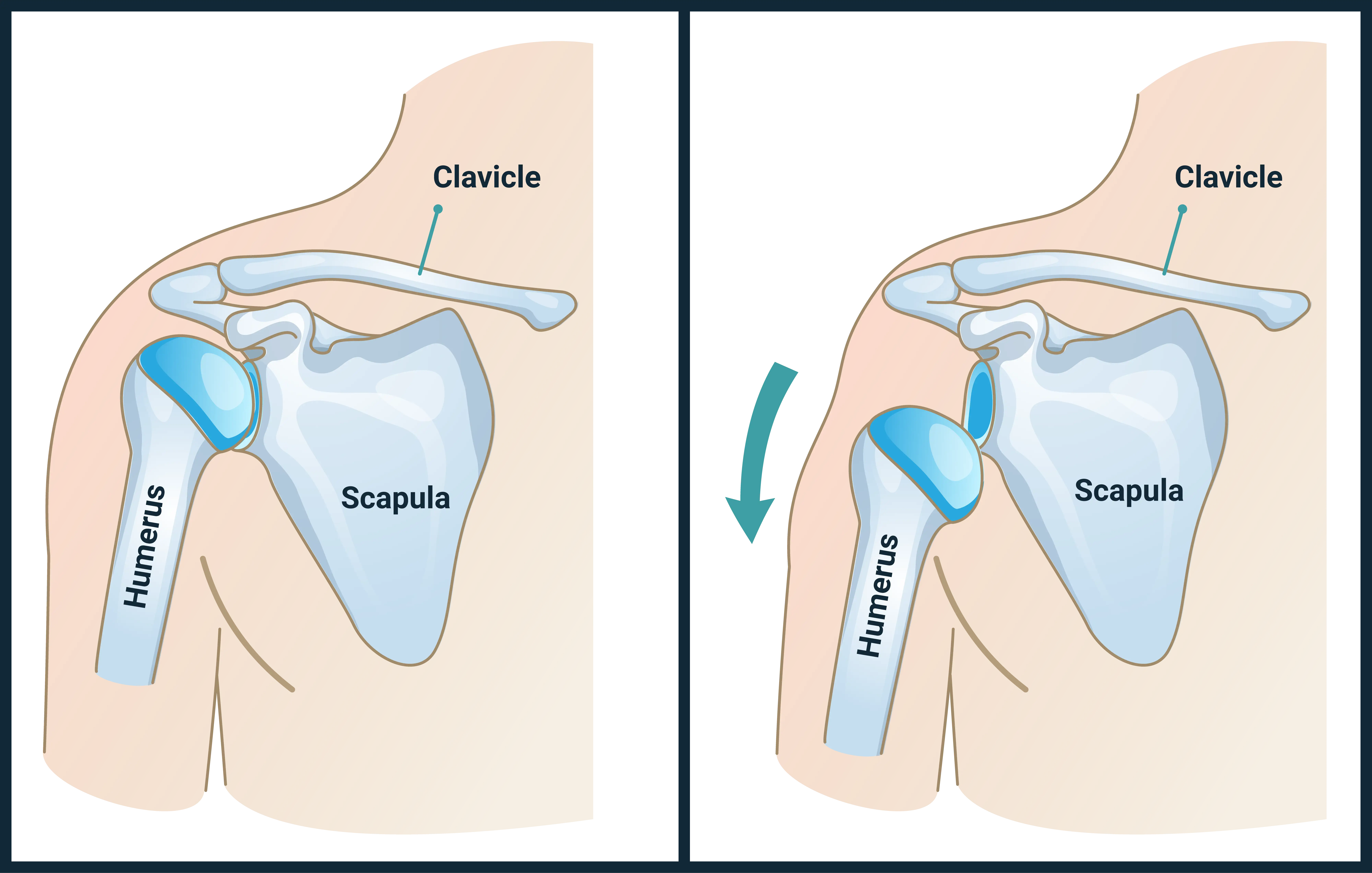
The shoulder is a ball-and-socket joint comprised of three main bones: the humerus (upper arm bone), the scapula (shoulder blade), and the clavicle (collarbone). The “ball” is the head of the humerus, and the “socket” is a shallow depression in the scapula called the glenoid. This unique anatomical structure allows for an extraordinary range of motion. However, this mobility comes at a cost: it also makes the shoulder highly susceptible to dislocation and other injuries.
A dislocated shoulder occurs when the head of the humerus is forced out of its normal position in the glenoid socket. This can be a partial dislocation, known as a subluxation, where the ball only partially comes out of the socket, or a complete dislocation, where the ball fully separates from the socket.
When a dislocation happens, it can stretch or tear the ligaments, tendons, and muscles that normally hold the joint in place. These soft tissues, along with the joint capsule (a fibrous sac enclosing the joint) and the labrum (a rim of cartilage around the glenoid that deepens the socket), are important for shoulder stability.
Damage to these structures can lead to chronic shoulder instability, making the joint more prone to future dislocations. The severity of the injury depends on the force involved and the extent of damage to these stabilizing structures.
Causes of a Dislocated Shoulder
Shoulder dislocations are predominantly caused by trauma, often involving a significant force that pulls, twists, or impacts the shoulder joint. Understanding the common scenarios that lead to this injury can help in prevention and early recognition.
One of the most frequent causes of shoulder dislocation is falls. This can include falling directly onto the shoulder, falling onto an outstretched arm, or falling from a height.
Sports injuries are another leading cause, especially in contact sports or activities that involve overhead arm movements. Sports such as football, rugby, hockey, basketball, and wrestling frequently expose athletes to collisions, tackles, or falls that can result in shoulder dislocation. Motor vehicle accidents can also cause shoulder dislocations.
Finally, a history of previous shoulder dislocations is a risk factor for future dislocations. Repeat dislocations may cause instability, which can make the shoulder more prone to re-dislocation with less force.
Symptoms of a Dislocated Shoulder
Recognizing the symptoms of a dislocated shoulder can prompt timely medical care. Intense pain is typically the most immediate and prominent symptom. The pain is usually sharp, severe, and localized to the shoulder area. It may be worsened by any attempt to move the arm or shoulder.
Additionally, a dislocated shoulder often presents with a noticeable change in the shoulder’s appearance. The normal rounded contour of the shoulder may be lost, appearing flattened, squared-off, or abnormally prominent. The arm may also appear longer or shorter than the uninjured arm, or it might be held in an unusual position.
Shortly after the injury, swelling around the shoulder joint is common as blood vessels and soft tissues are damaged. Bruising may develop hours or days later, appearing as discoloration around the shoulder and upper arm. Other possible symptoms include limited range of motion, numbness or tingling, and weakness.
Possible Treatments: Non-Surgical
When a shoulder dislocation occurs, the typical priority is to safely return the humeral head to its proper position within the glenoid socket. This process, known as reduction, is almost always performed by a trained medical professional. Following reduction, non-surgical treatments focus on pain management, immobilization, and rehabilitation to restore function and prevent recurrence.
Closed Reduction
Closed reduction involves specific maneuvers performed by a doctor to gently guide the humeral head back into the glenoid socket without making an incision. This procedure may be performed under anesthesia, especially if the patient is in severe pain or if muscle spasms are making reduction difficult.
Immobilization
After successful reduction, the shoulder is typically immobilized using a sling. The purpose of immobilization is to keep the arm in a position that supports the stretched or torn ligaments, tendons, and joint capsule in healing. The duration of immobilization varies depending on factors such as the patient’s age, the severity of the dislocation, and whether it’s a first-time or recurrent dislocation.
Pain Management
Pain relief is a key component of non-surgical treatment. Immediately after the injury and reduction, ice packs are often applied to reduce swelling and pain. Along with ice, nonsteroidal anti-inflammatory drugs (NSAIDs) are commonly used.
Physical Therapy and Rehabilitation
Once the initial pain and swelling have subsided and the shoulder has had some time to heal in immobilization, physical therapy becomes a core part of non-surgical treatment. The goals of physical therapy are to restore range of motion, strengthen the muscles, and improve balance and proprioception. The physical therapy program is tailored to the individual’s needs and progresses through various phases, from gentle passive movements to active strengthening and functional exercises.
Possible Treatments: Surgical
While non-surgical treatment is often the first-line treatment for dislocations, surgery may be recommended in certain situations. Surgical intervention aims to repair damaged tissues, restore stability to the shoulder joint, and reduce the risk of recurrent dislocations. The decision for surgery is typically based on factors such as the patient’s age, activity level, the number of previous dislocations, and the extent of damage to the soft tissues or bone.
Types of Surgical Procedures
Several surgical techniques can be employed to stabilize a dislocated shoulder, often performed arthroscopically or through open surgery, depending on the complexity of the injury.
Shoulder arthroscopy is a minimally invasive procedure and a common surgical approach for damage caused by dislocations. In arthroscopic procedures, small incisions are made around the shoulder, through which a tiny camera (arthroscope) and specialized instruments are used.
The surgeon can then visualize the inside of the joint and repair damaged structures. In cases where arthroscopic repair is not feasible, open surgery may be necessary, which involves a larger incision. An experienced shoulder surgeon can evaluate the injury and help guide the most appropriate treatment plan.
Recovery Process After a Dislocated Shoulder
Whether the treatment is non-surgical or surgical, the ultimate goal is to restore full function, strength, and stability to the shoulder while minimizing the risk of future dislocations. The recovery timeline can vary significantly based on the individual’s age, the severity of the injury, the presence of associated damage (e.g., fractures, severe soft tissue tears), and the chosen treatment approach.
Immediate Post-Reduction/Post-Surgery Phase
This initial phase generally focuses on protecting the healing tissues, managing pain and swelling, and preventing stiffness. For both non-surgical and surgical cases, the shoulder will typically be immobilized in a sling or brace.
During this period, pain management and rest are prioritized. While the shoulder is immobilized, the physical therapist may recommend gentle exercises for the hand, wrist, and elbow to maintain circulation and prevent stiffness in these joints.
Early Motion and Strengthening Phase
Once the initial healing has progressed, the focus shifts to gradually restoring range of motion and initiating gentle strengthening. The sling is usually discontinued during this phase, though it may still be used for comfort or protection in certain situations. Your physical therapist will typically begin to guide active range of motion, strengthening, and proprioception exercises.
Advanced Strengthening and Return to Activity Phase
This phase may be dedicated to building strength, endurance, and power, preparing the individual for a safe return to daily activities, work, and sports. A safe return to activity is guided by your surgeon and physical therapist, with criteria typically including range of motion, symmetrical strength compared to the uninjured side, and completion of functional tests. It’s important to avoid returning to high-risk activities too soon, as this may increase the risk of re-dislocation.
Summary
A dislocated shoulder is a painful injury that often demands prompt and appropriate medical attention. Recognizing the key symptoms, including intense pain, visible deformity, limited movement, and potential numbness or tingling, is essential for seeking timely care and preventing further complications.
Treatment strategies for a dislocated shoulder are tailored to the individual, considering factors like age, activity level, and the extent of tissue damage. Non-surgical approaches, centered around closed reduction, immobilization, pain management, and a comprehensive physical therapy program, are often effective for first-time dislocations. However, for some cases, surgical intervention may be recommended to restore stability and prevent future episodes.
By understanding the nature of this injury and committing to the recovery process, individuals can support their healing journey and reduce the risk of re-injury.
Frequently Asked Questions
What should I do immediately if I think I’ve dislocated my shoulder?
If you suspect a shoulder dislocation, it is generally important to seek medical attention. Do not attempt to put the shoulder back into place yourself, as this may cause further damage to nerves, blood vessels, or surrounding tissues. Immobilize the arm as best as you can and apply ice to reduce swelling and pain.
How long does it take to recover from a dislocated shoulder?
Recovery time varies significantly depending on the severity of the dislocation, whether it’s a first-time injury or recurrent, and if surgery was required. For non-surgical cases, initial recovery with immobilization and physical therapy can take several months. If surgery is performed, full recovery, including extensive rehabilitation, may take longer.
Is surgery always necessary for a dislocated shoulder?
No, surgery is not always necessary. Many first-time shoulder dislocations can be successfully treated with closed reduction, immobilization, and physical therapy. Surgery is typically considered for recurrent dislocations, significant structural damage, or in active individuals who are at high risk of re-dislocation.
Can I prevent shoulder dislocations?
While not all dislocations are preventable, especially those due to high-impact trauma, you can reduce your risk. Strengthening the muscles around your shoulder, particularly the rotator cuff and scapular stabilizers, can support joint stability. Maintaining good posture, avoiding risky movements, and using proper technique during sports or physical activities are also helpful strategies.



