For individuals experiencing persistent shoulder pain and limited mobility, particularly due to complex conditions like severe rotator cuff tears or advanced arthritis, reverse total shoulder arthroplasty offers a promising option. In this post, we aim to explore reverse total shoulder arthroplasty, explaining what it is, when it is recommended, and what patients can expect during the recovery process.
Key Takeaways
- Reverse total shoulder arthroplasty is a specialized shoulder replacement surgery where the ball and socket components are reversed, allowing the deltoid muscle to power arm movement when the rotator cuff is severely damaged.
- This procedure may be recommended for patients with rotator cuff tear arthropathy, irreparable rotator cuff tears, or complex shoulder fractures.
- The main objectives of reverse total shoulder arthroplasty are to reduce pain, restore functional arm movement, and improve quality of life.
Understanding Reverse Total Shoulder Arthroplasty
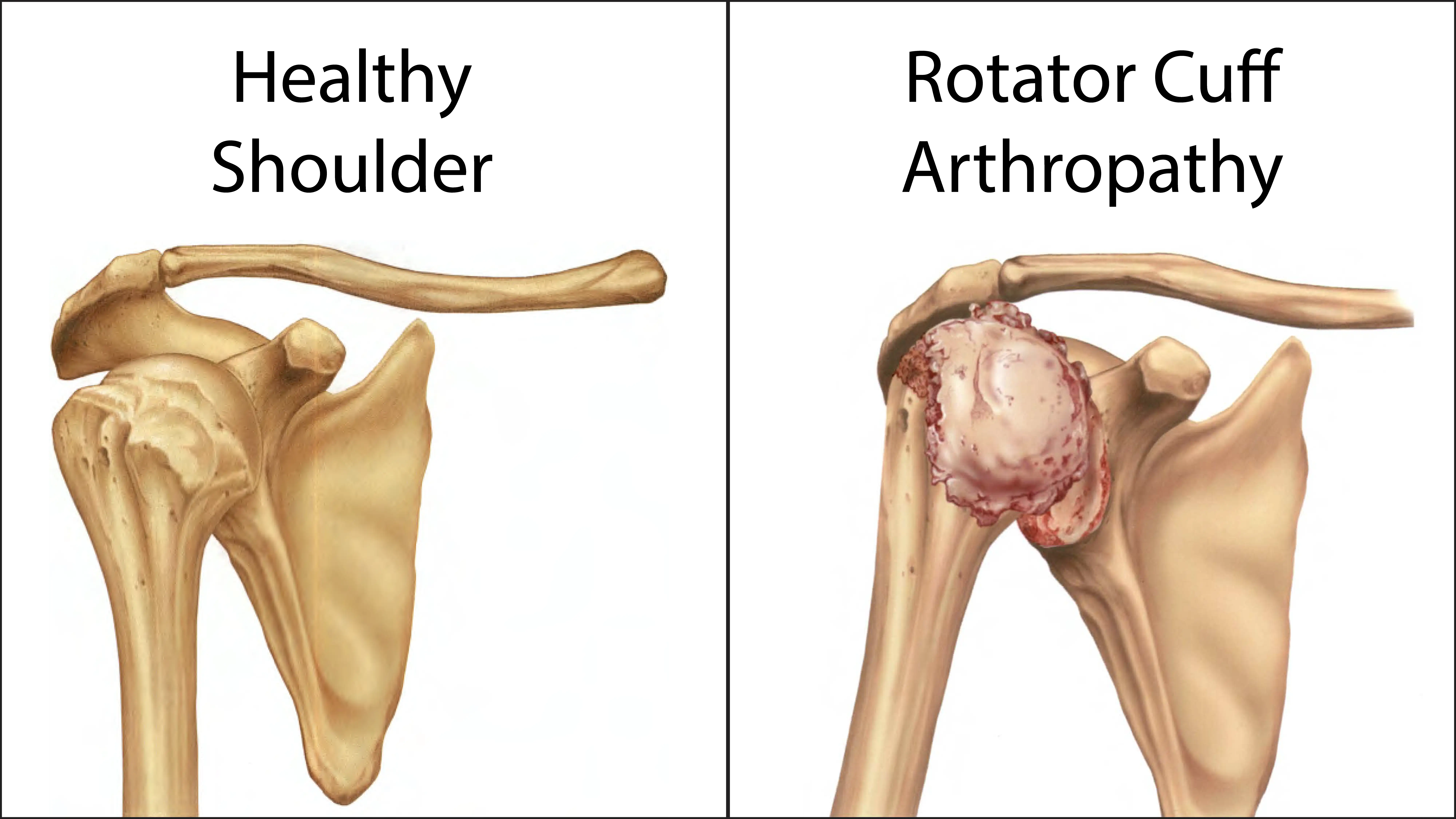
To understand the reverse shoulder replacement procedure, it’s helpful to first grasp the basic anatomy of the shoulder and how a traditional total shoulder replacement works. The shoulder is a complex ball-and-socket joint, where the head of the humerus (upper arm bone) fits into a shallow socket on the scapula (shoulder blade) called the glenoid. This design allows for an incredible range of motion, but it also relies heavily on a group of four muscles and their tendons, collectively known as the rotator cuff, for stability and movement.
In a traditional total shoulder replacement surgery, the damaged humeral head is replaced with a metal ball, and the glenoid socket is covered with a plastic component. This mimics the natural anatomy of the shoulder, and its success often depends on a healthy, functioning rotator cuff to power the arm’s movement.
Reverse shoulder replacement, however, takes a fundamentally different approach. As its name suggests, the ball and socket components are reversed. A metal ball is fixed to the shoulder blade where the natural socket used to be, and a plastic socket is attached to the top of the humerus. This design alters the biomechanics of the shoulder joint.
The primary reason for this reversal is to compensate for a severely damaged or non-functional rotator cuff. In a healthy shoulder, the rotator cuff muscles lift and rotate the arm. When these muscles are torn beyond repair, or when the joint is severely arthritic due to rotator cuff deficiency (a condition known as cuff tear arthropathy), a traditional replacement would likely prove inadequate because there are no intact muscles to move the new joint.
By reversing the ball and socket, reverse shoulder replacement shifts the center of rotation of the shoulder joint. This allows the large deltoid muscle, which covers the outside of the shoulder, to become the primary muscle responsible for lifting and moving the arm.
When is Reverse Total Shoulder Arthroplasty Recommended?
Reverse shoulder replacement is not a first-line treatment for all shoulder pain but rather a solution for specific, complex conditions where traditional treatments, including anatomic total shoulder replacement, are unlikely to succeed. An experienced shoulder surgeon can evaluate the condition and help guide if reverse shoulder replacement might be the right option for you.
Rotator cuff tear arthropathy is a common indication for reverse shoulder replacement. It occurs when a large, long-standing, and irreparable rotator cuff tear leads to significant arthritis. Patients often experience severe pain, weakness, and extremely limited shoulder motion.
Even without advanced arthritis, a massive rotator cuff tear that cannot be surgically repaired can severely compromise shoulder function and cause chronic pain. If conservative treatments like physical therapy and medication fail to provide relief, surgery may be considered.
Additionally, severe fractures can be particularly challenging to treat, especially in older patients with diminished bone quality. In such cases, reconstructing the fracture may be difficult, and the risk of complications like avascular necrosis (bone death due to loss of blood supply) is high. Reverse shoulder replacement may provide a solution by replacing the fractured bone with prosthetic components.
The Surgical Procedure: What to Expect
The procedure usually takes a few hours, and while the specifics may vary based on individual patient anatomy and the surgeon’s technique, the general steps involve the following:
- Incision and Exposure: The surgeon makes an incision, usually on the front or top of the shoulder, to access the shoulder joint.
- Preparation: The glenoid and humerus are prepared to receive the prosthetic components. Damaged bone and cartilage are removed, and the sites are shaped.
- Implant Placement: The prosthetic components are inserted and attached.
- Stability Check: The stability and range of motion of the new joint are checked. Adjustments may be made to ensure optimal positioning.
- Closure: The surgeon irrigates the surgical site, closes the incision layer by layer, and applies a sterile dressing. A drain may be placed temporarily to collect any excess fluid.
Following the procedure, the patient will be moved to the recovery room. The patient may be discharged or kept in the hospital overnight, depending on their recovery progress and overall health.
The Recovery Process
Immediately after surgery, the arm will be placed in a sling or immobilizer to protect the healing tissues and the new joint. Pain and swelling are common during this time, and effective pain management strategies, including oral medications, may be employed to ensure comfort.
Physical therapy typically begins shortly after surgery. The initial focus is on protecting the surgical repair and preventing stiffness. During this phase, exercises are primarily passive, meaning the therapist moves the arm without the patient actively engaging their shoulder muscles. This helps to maintain range of motion without stressing the healing tissues.
As healing progresses, the rehabilitation program will gradually advance. Active range of motion exercises are introduced. The goal is to slowly regain more independent movement. Strengthening exercises for the deltoid muscle and surrounding scapular stabilizers may also begin, focusing on light resistance and controlled movements.
Return to Activity and Long-Term Recovery
By six months to a year post-surgery, many patients can return to most daily activities, though timelines vary. The recovery focus generally shifts to sport-specific or work-specific training, if applicable, and continued strengthening to maximize the long-term outcomes.
Throughout the recovery process, adherence to the physical therapy program is key. Consistency, patience, and open communication with the healthcare team are factors in achieving the best possible outcome after reverse shoulder replacement.
Summary
Reverse total shoulder arthroplasty represents an advancement in orthopedic surgery, offering a potential solution for individuals with complex shoulder problems that were once considered untreatable. By redesigning the shoulder joint, this procedure aims to provide pain relief and functional restoration, particularly for those with severe rotator cuff damage. If you are struggling with chronic shoulder pain and limited mobility, and have been told that a traditional shoulder replacement is not an option, consider consulting a shoulder specialist to see if reverse shoulder replacement may be a possible treatment strategy for you.
Frequently Asked Questions
Will I have any restrictions after reverse shoulder replacement surgery?
There may be some restrictions, particularly in the early stages of recovery. Your surgeon will provide specific guidelines, but generally, you will be advised to avoid heavy lifting, high-impact activities, and certain sports that could put excessive stress on the implant. The goal is to protect the new joint and ensure its longevity.
How much pain can I expect after the surgery?
Pain management is a priority after reverse total shoulder arthroplasty. You will receive a combination of strategies to control pain and discomfort. While some pain is expected in the immediate post-operative period, it can typically be managed and will gradually subside as you heal. Many patients experience meaningful pain relief after surgery.
How is reverse shoulder replacement different from an anatomic total shoulder replacement?
The key difference lies in the design and the muscles used to power the arm. In an anatomic replacement, the implant mimics the natural ball-and-socket anatomy, and the rotator cuff muscles are prioritized for movement. In a reverse replacement, the ball and socket are reversed, allowing the deltoid muscle to take over the function of a damaged rotator cuff. This makes reverse total shoulder arthroplasty a potentially suitable option for patients with severe rotator cuff deficiency.



